The unexplained rise of cancer among millennials Scientists are not sure why
When Paddy Scott developed agonising stomach pains in 2017, the possibility of cancer never entered his head. The British expedition photographer and film-maker, whose work often took him into rugged or dangerous terrain, was just 34 years old and prided himself on his physical fitness.
After his GP referred Scott to hospital for a colonoscopy, the clinician who administered it asked if he would take part in a trial of a new blood test designed to detect tumours. The invitation struck him as strange. “I remember thinking, yes but I’ll be the kind of ‘control’ that doesn’t have it,” Scott says. Later he received the devastating news that he had advanced bowel cancer which had spread to his liver.
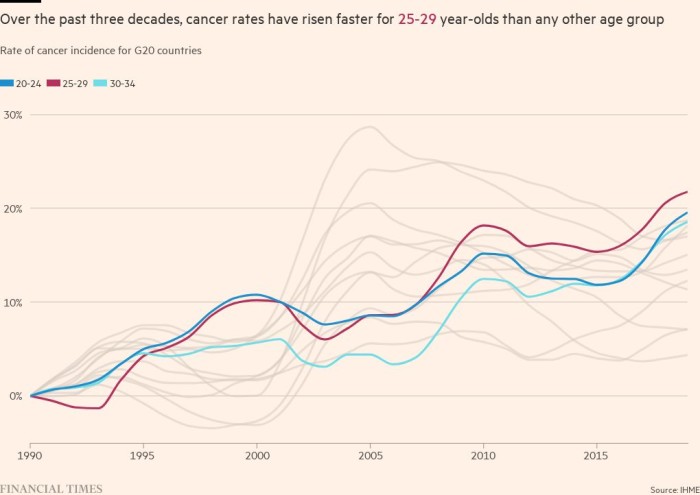
Researchers have no definitive explanation for why people in the prime of life seem to be markedly more vulnerable to the disease than their counterparts in earlier generations.
The trend has economic, clinical and social implications. For cancer doctors on the frontline, the rise in such cases is becoming an inescapable and worrying aspect of their practice. Shahnawaz Rasheed, the surgeon in charge of Scott’s treatment at the Royal Marsden, a renowned London cancer hospital recalls a two-week period a couple of years ago when he operated on four women under 40. Another recent patient was a super-fit, international sportswoman in her 30s.
Cancer often develops over decades — people can harbour slow-growing tumours for years — so for those diagnosed in their twenties, thirties and forties “some of the risk factor exposures may have happened when they were a baby or even in utero”, says Prof Shuji Ogino, an epidemiologist at the Harvard TH Chan School of Public Health who is part of the CRUK/NCI research initiative.
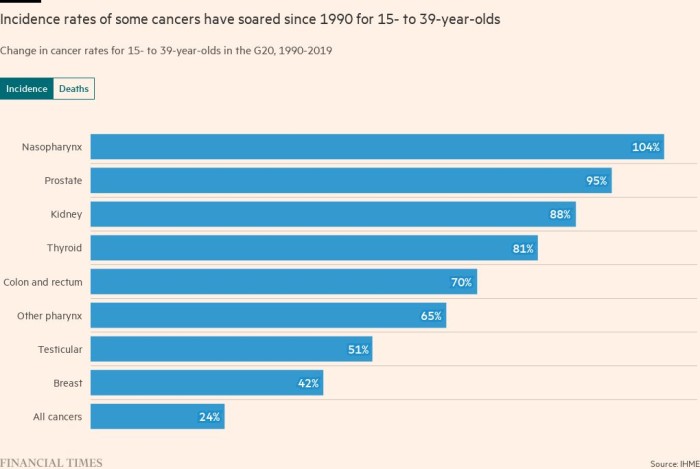
The fact that the biggest increases in cancer in the young have been in gastrointestinal varieties — colorectal as well as in the oesophagus, stomach, pancreas, bile duct, liver and gallbladder — bolsters the case for a link with diet.
Some other cancer types increasingly seen in younger people, such as breast, kidney and endometrial cancers, plus the blood cancer myeloma, may be affected both by obesity and the condition of the microbiome even though they lack an obvious link to the digestive system, Ogino says.
Additionally, antibiotic use and medications more generally can affect an individual’s microbiome, sometimes referred to as their “bacterial fingerprint”.
Ogino points out that during the second half of the 20th century the range of medicines available to treat multiple conditions substantially increased. New anti-obesity medicines are a recent example. “The effect really remains unknown what they all do in the long term,” Ogino says.
The link to the microbiome is still circumstantial, he emphasises. He points to other changes that occurred from the 1950s onwards: more sedentary lifestyles, changes to sleep patterns and repeated exposure to bright light at night that can affect circadian rhythms and metabolism. “All these changes are happening in a really parallel way so it’s hard to tease out the culprit. There are likely multiple culprits which work together,” he says.
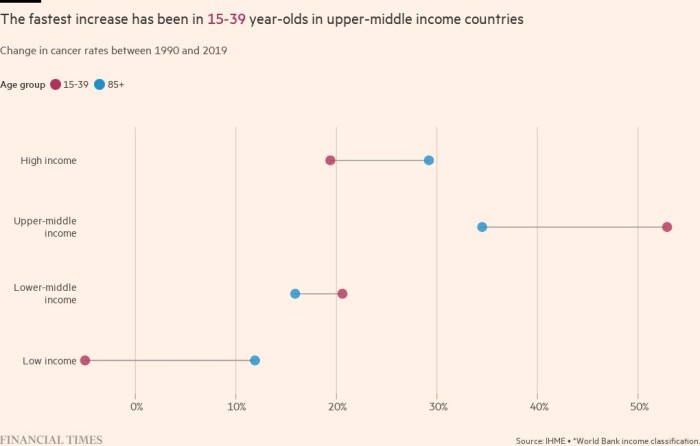
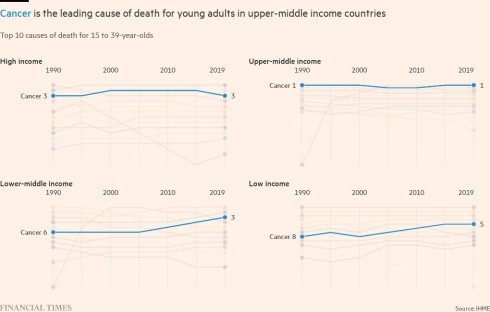
The rise in cases in wealthy western countries now looks set to find a belated, but resounding, echo in poorer countries where these societal changes happened decades later than in the US or the UK. The FT’s research shows that between 1990 and 2019, cancer rates for 15- to 39-year-olds increased significantly faster in upper-middle income countries, such as Brazil, Russia, China and South Africa, compared to high-income countries: by 53 per cent compared to 19 per cent.
Valerie McCormack, an epidemiologist who has studied disease patterns in cancer in low and middle income countries, where infectious diseases have long posed the biggest health burden, suggests a number of factors could be increasing rates of non-communicable diseases, including cancer, in the Brics and other developing nations.
Women in these countries are having fewer children overall, and at later ages, meaning they spend a shorter period of their lives breastfeeding compared with previous generations. Having a larger family — typically leading to an extended period of breastfeeding — and giving birth for the first time at a young age are factors known to confer protection against breast cancer.
“These changes do have many benefits for women, but they do place them at greater risk of breast cancer,” says McCormack, who is deputy branch head for environment and lifestyle epidemiology at the International Agency for Research on Cancer, part of the World Health Organization.
Similarly, an increase in smoking and alcohol use evident in some developing countries, mostly in men, is “narrowing the gap in cancer risk” between rich and poorer nations, while the adoption of a more westernised diet, obesity and lower physical activity were implicated in the growth of colorectal cancer cases, McCormack adds.
But she cautions: “These are epidemiological and lifestyle transitions which will be contributing to increasing rates of specific cancers” — but they are unlikely to tell the full story. “Some of the rises are so very recent that the research hasn’t been done to exactly pinpoint all of the driving factors,” she says.
Spotting ‘red flags’
The rise in early onset cancer is not simply a concern for health systems. It is a problem for economies too. Those who survive the disease are at greater risk of long-term conditions such as infertility, cardiovascular disease and secondary cancers, researchers say, threatening more costly healthcare burdens in future.
Simiao Chen, head of the research unit for population health and economics at the Heidelberg Institute of Global Health and an adjunct professor at Peking Union Medical College, led a team which earlier this year calculated that the estimated global cost of cancer from 2020 to 2050 would be $25.2tn at constant 2017 prices. This, the researchers concluded, was “equivalent to an annual tax of 0.55 per cent on global gross domestic product”.
“If the trend is getting younger then the economic burden will be much heavier because we are losing people in the working age population who can contribute to economic growth,” Chen says. Cancer survivors might not be able to recapture their previous productivity levels, she suggests. “So it will reduce the quantity and the quality of labour”, she adds.
Recognising that early onset cancers are becoming more common, some clinicians would like to see a reduction in the age of eligibility for screening programmes, most of which take effect only in later middle age.
In England, for example, home bowel cancer testing kits are sent out when patients reach 60. Last month, the US Preventive Services Task Force, an independent body made up of national experts, suggested that the age for breast screening should be lowered to 40. In 2021, the same group argued that colorectal screening should begin at 45.
As health systems around the world struggle with a mismatch between demand and resources made worse by the pandemic, mounting a compelling case for the necessary expenditure may prove harder. A “national dialogue” about priorities may be needed given the rising proportions of under-50s developing cancer, Rasheed, the Royal Marsden surgeon, says.
Some scientists say they have identified differences in the molecular structure of cancers in younger people, pointing to the potential need for specific treatments aimed at this group.
Tomotaka Ugai, a research fellow in epidemiology at Harvard’s Chan School who led a study into rising rates of early onset cancer which drew international attention to the trend in 2021, says that for many cancer types such as breast, colorectal, endometrial, multiple myeloma, pancreatic and prostate, “early onset cancers have more aggressive clinical features”.
A related question is whether the causes of early onset cases are different to those diagnosed at older ages. Ugai says: “We assume that many risk factors overlap between early onset and later onset, but we don’t know if risk factors completely overlap . . . so we need to conduct more research.”
Some clinicians believe that equally important is the fact that cancers have often reached a more advanced stage in a younger person before they are diagnosed. They believe doctors need to be on the alert for cancer in a 20- or 30-something, recognising this can no longer be considered an outlandish prospect.
Rasheed, who regularly lectures to GPs about the importance of spotting cancer “red-flag” signs early, says studies have shown that younger people “may have been seen by five or six clinicians, before being referred for specialist investigations, diagnosis and treatment”. The same symptoms in someone 30 years older would have probably rung immediate alarm bells. The delayed diagnoses may also reflect a lack of awareness among younger people of the symptoms they should look out for, he suggests.
“I’ve heard and seen a lot of horror stories about younger people who, by the time they come in [to hospital] have got quite locally advanced or metastatic disease. And there may have been a window [to find and treat the cancer] earlier,” he says.
Scott recalls that, after his GP referred him to a central London hospital for tests, “apparently they said to her, ‘This isn’t urgent, he’s 34, he’s clearly in very good health’. She pushed and pushed and eventually managed to get me in.”


The question preoccupying researchers and clinicians is whether the rise in cases over the past few decades represents the tip of a much larger epidemiological iceberg.
In their research paper, Ugai and his fellow researchers warned of the possibility that those who are currently children, adolescents and young adults might have higher risks of cancer throughout their lives compared to older generations.
And it may not stop at cancer. The same risk factors may predispose them to conditions such as diabetes and inflammatory bowel disease, the scientists said, suggesting a permanently higher chronic disease burden in the future unless action is taken to spur healthier ways of living and eating, and to reform the way that food is produced and distributed.
While the prevalence of smoking, a key cause of cancer, has decreased in many parts of the world over the past few decades, obesity, physical inactivity and other risk factors have increased, Ugai notes. “So there is a trade off but we can speculate that [early onset cancer] cases will continue to grow for the foreseeable future,” he says.
For younger people like Scott who were previously healthy and fit, cancer can seem like the ultimate misfortune, the shortest of straws. As he copes with his diagnosis, Scott resists asking “why me?” He has started a masters degree in environmental politics and policy and became a father 11 months ago when his partner, Hen, gave birth to their son, Osprey.
But he inevitably reflects on what might have been. “I’d spent 10 years trying to break into wildlife film-making. And then just as I started [cancer] treatment, I started getting job offers and had to turn them down.
“I can’t help but think, ‘What would my life be like if I didn’t have to be going through all this?’”
This story originally appeared on: Financial Times - Author:Amy Borrett

























