Cradle to grave: is Britain’s NHS broken?
When plans for King Charles’s coronation were announced, one detail was especially revealing about the country over which he reigns. At the centre of the celebrations will be choirs of NHS workers, a reminder that when the UK wants to showcase the best of itself for a worldwide audience, it turns to its health service.
In July, it will be 75 years since the UK founded the tax-funded system of free care that, as a former finance minister once remarked, is the closest thing the multicultural nation has to a national religion.
Each “big birthday” has offered a chance for reflection about its future, and scarcely one has passed without the occasional prediction of its imminent demise. But, fittingly perhaps as it enters later old age, never before have its frailties been more exposed and the mismatch between resources and demand so apparent.
Founded in 1948 by Clement Attlee’s Labour government, the brainchild of his health minister Aneurin Bevan, the NHS was designed to improve heath outcomes for a population depleted by war and suffering ill health based on the 1942 blueprint for a more just society drawn up by the social reformer William Beveridge.
Before the service was set up, healthcare provision for those who lacked means was patchy. As late as the 1930s, more than 80 per cent of children in London and Durham showed symptoms of rickets, a sign of preventable malnutrition, according to Prof Roberta Bivins, a historian at Warwick university.
Cradle to grave: can the NHS be fixed?

The second of the FT’s two-part series looks at ways the health service can be reformed if it is to survive a further 75 years
Part 2 coming tomorrow
The level of ill health endured by many was made clear by Dr John Marks, who qualified on the first day of the new service and went on to lead the British Medical Association 40 years later. Quoted by public policy expert Nicholas Timmins, in his history of the welfare state, The Five Giants, Marks said: “There were women with prolapsed uteruses literally wobbling down between their legs that had been held in place with cup and stem pessaries . . . You would have men walking round with trusses holding these colossal hernias in.”
The chosen form “fitted within their particular model of postwar planning ideology . . . you needed the health system to be plugged into the state”, he said.
The new service established a tripartite structure, divided between general practitioners, hospitals and community services, that remains essentially unchanged. GPs are still, for the most part, independent contractors running their practices like small businesses, a concession Bevan agreed as the price of overcoming their resistance to the new nationalised health system.
Bevan and Attlee had assumed that unfettered access to healthcare would improve the health of the population to such an extent that the cost of providing it would fall. However, neither anticipated how longer life expectancy and medical advances would radically change the costs and form of healthcare.
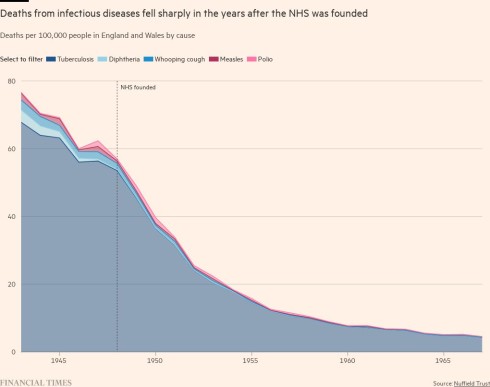
Referrals to specialists were rare in the 1940s when most care was delivered by GPs, established from the start as gatekeepers to the wider system. While stays in hospital were far longer than they are now, they were often principally for convalescence from infectious diseases.
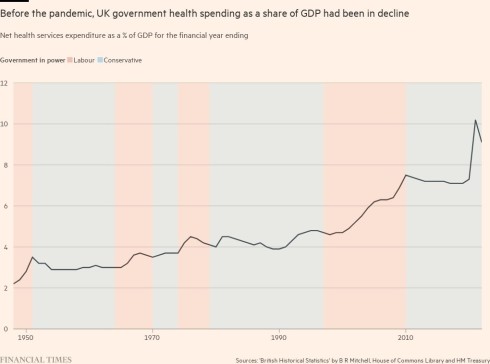
The initial cost estimates were also wildly short of the sums that turned out to be required. Its first year of operation cost £305mn, far outstripping the £170mn originally estimated in Beveridge’s 1942 report. The proportion of GDP absorbed by the NHS has risen from 2.24 per cent in 1948 to 9.17 in 2022.
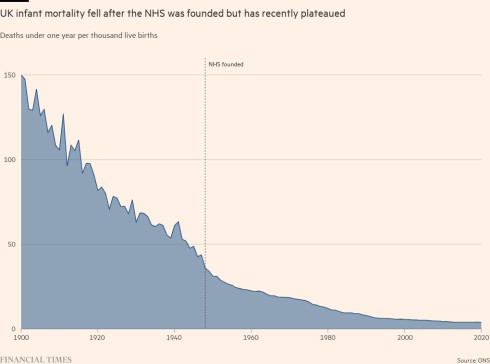
As the public felt the impact of the service, its popularity soared. Levels of infectious disease fell precipitately. Life expectancy, which had been on a rising curve since the beginning of the century continued its upward course.
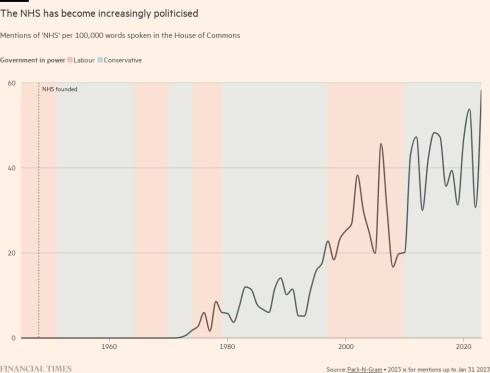
Yet, although the nation had by the 1950s warmed to the security the service brought, health for years was not prominent in political parties’ manifestos. It was not until the 1980s that the notion of the NHS as a repository of national values really took root, obliging any politician seeking national office to pay obeisance to it. This mindset frequently led to claims that only the election of one party over another could “save” the NHS.
Seaton suggests this process was the result of a conscious effort by left-leaning supporters, not least in the media, who perceived the service’s core model to be under threat during Margaret Thatcher’s premiership. A rash of television features about the horrors of US healthcare helped to shape the debate, implying any departure from the current model would subject Britons to the same iniquities as Americans.
In 1998, the anthropomorphic notion of the NHS’s “birthday” as an occasion for national thanksgiving was introduced for the first time, and included a special 50p coin. In 2012, Danny Boyle’s much-feted opening ceremony for the London Olympics, which sought to distil modern Britain for the world, featured a parade of dancing NHS nurses and sick children. By 2018, when Theresa May led celebrations of its 70th, the soft-focus approach had been uncritically adopted by the Conservatives, too.

The soaring costs of a national treasure
The decision to freight the NHS with meaning, and set up a narrative in which it must be protected even when other areas of public spending were not, has had a crucial impact on the way British state expenditure has evolved over the past 50 years.
Spending on the NHS has swallowed an ever-greater share of the public purse, as an ageing and growing population has irrevocably changed the demands on the system since the days when most barely lived long enough to collect their state pension, let alone develop the chronic diseases of old age — dementia, diabetes — that now come close to overwhelming its budget.
Since 1979-80, the health department’s budget has grown more than fourfold in real terms from £35bn to £164bn, expressed in 2021-22 prices, and it has doubled its share of the GDP pie, according to the Nuffield Trust, a think-tank.
Initially the vast sums the health service consumed did not have a big impact on other important areas of public expenditure. Anita Charlesworth, director of research at the Health Foundation, a charity, said this rising share of overall public spending was “accommodated without the need for substantial tax increases by a change in what the rest of the state was doing”: first the privatisation of the utilities and secondly the end of the cold war, which freed up funds from defence spending.
But as the share of public expenditure taken by the NHS has soared so too has politicians’ desire to find ways of ensuring that this bounty is better spent through multiple attempts at “reform”.
Nigel Edwards, chief executive of the Nuffield Trust, said that, in contrast to the often-touted idea that the NHS is untouchable due to the reverence in which Britons hold it, it is in fact the most reorganised health system in western Europe “by a country mile”.
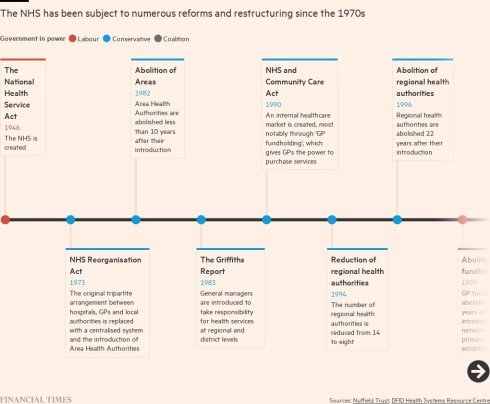
The result has been an alphabet soup of acronyms, and some sharp strategic shifts as different politicians imposed their own visions on the service — from competition to collaboration, from tighter central control to increased devolution — but few obvious associated improvements to public health. He ascribes this to an ingrained NHS view that its primary accountability is to the secretary of state, not the patients it serves.
But Richard Sloggett, previously an adviser to former Conservative health secretary Matt Hancock, who now runs a health consultancy, argued that politicians, unable to risk alienating the electorate with any fundamental changes to the service’s funding model, had instead sought organisational change as a less politically dangerous way of attempting to improve its productivity.
However, even more than the health department or Number 10 itself, there is one bastion of government that has shaped the history and direction of the NHS: the Treasury, which under the British model exercises a rare — perhaps unique — degree of financial sway over the level of health service funding.

Even countries whose health systems are primarily funded from the national tax base like the NHS — the Scandinavian countries, for example — have a “countervailing tier” of regional control that ensures they are not entirely in thrall to a central finance ministry, Edwards said.
He laments the Treasury’s inability to invest for the longer term, and says few counterparts around the world take so narrow a view of their remit to balance the books even at the expense of the nation’s welfare.
The only time in recent decades that the NHS has been relatively amply funded — producing huge improvements in waiting times and a doubling of patient satisfaction — was during the New Labour years, 1997-2010.
Edwards points out this was the only time that the Treasury was circumvented; in January, 2000 Tony Blair used an appearance on a Sunday morning political programme to announce that he was raising spending on the NHS to the European average by the end of the following parliament. His chancellor, Gordon Brown had not been told in advance. Afterwards a splenetic Brown reportedly told Blair that he had “stolen my fucking budget”.

The repercussions of austerity
After years of largesse, much of the state of the NHS today can be traced to the impact of 10 years of post-financial crisis austerity that began under David Cameron’s coalition government in 2010. It was not simply the amount of funding it received, but its distribution, and the impact on the rest of Whitehall that made the difference — and it was in part the need to keep very public faith with a beloved institution that sowed the seeds of some of the current problems.
Cameron, anxious to be seen to show fealty to the NHS, which had cared for his severely disabled son and to which he had a genuine commitment that some Tory predecessors had lacked, decreed that the NHS must be protected with real terms increases.
However, other departments, such as criminal justice and local government, suffered deep cuts “in an attempt to create the headroom for the health service to grow without taxes needing to rise”, Charlesworth said.
Budget streams with a crucial impact on the health of the nation — infrastructure, preventive health, medical education and, perhaps most crucially, local government, which funds social care — also faced real term cuts during his administration.
The result, said Professor Sir Michael Marmot, a global expert in the impact of “social determinants” such as housing and nutrition on health, is that in the past decade improvements in life expectancy first slowed, then reversed — a process exacerbated, but not caused, by the pandemic, he added.
“There was a sharp interruption in the curve in 2010,” he said. “Life expectancy stopped improving at the same rate, health inequalities increased. Life expectancy for the poorest people went down.”
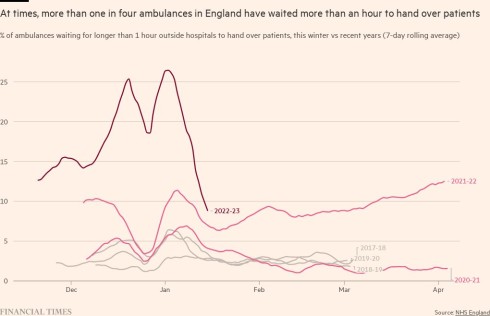
The NHS is currently living through its worst ever winter. Ambulance response times and waits in A&E departments in England are at record levels, with help taking, on average, more than 90 minutes to arrive even to suspected heart attack and stroke victims.
In December more than 54,500 patients waited over 12 hours in emergency departments after clinicians decided they needed a hospital bed. That is the highest-ever number and almost treble the figure for May last year.
But as politicians consider how to arm the NHS for the future, they must reckon with national sentiment as well as the day to day reality of a health service under unimaginable pressure, just as they have done for the past 75 years.
The latest set of British Social Attitudes findings, released last year, showed satisfaction with the service falling to its lowest level since 1997. “Confidence in the NHS being there for people is dropping. But yet at the same time, we’re not seeing any shift in support for the principles,” said Dan Wellings, a senior fellow at the King’s Fund, who specialises in public attitudes to health and social care.
“The public does not want a different model. They just want this one to work.”
He added that as recently as last year — with every NHS metric flashing red — an Ipsos poll asking what made people proudest to be British showed “the NHS . . . is still the top answer by some considerable margin”.
In future, however, trade-offs will become increasingly painful for other areas of vital state spending, Charlesworth suggested. As well as the NHS, social care and pensions are all likely to increase as a share of GDP as the baby boomer generation reaches old age. “There is very little other activity undertaken by the state that you could look to cut,” she warned.
But with a historian’s long view, Bivins recalls previous crises, when the parlous state of the health service had prompted doom-laden predictions about its capacity to survive. “History is not a predictive science, but I would say we have seen all this before,” she said.
She suggests the rich symbolism of the NHS may be its best guarantor of long term survival.
“The establishment of the NHS has been called ‘the least sordid political act’,” she said. “And I think that that’s really still true. People still look at it and say ‘we did this thing for everyone’.”
Additional reporting by Federica Cocco and Ella Hollowood
This story originally appeared on: Financial Times - Author:Ella Hollowood

























